Which of the Following Is Prohibited by Medicare
But they may also offer extra benefits that cover some of the gaps listed above. 1 The patient must first be admitted to an acute care hospital for a minimum of 3 days 2 The patient must have a documented medical need for skilled care and services 3 The patient must meet verified minimum financial hardship requirements 4 The patients stay must be no more than 100 days in a calendar year.
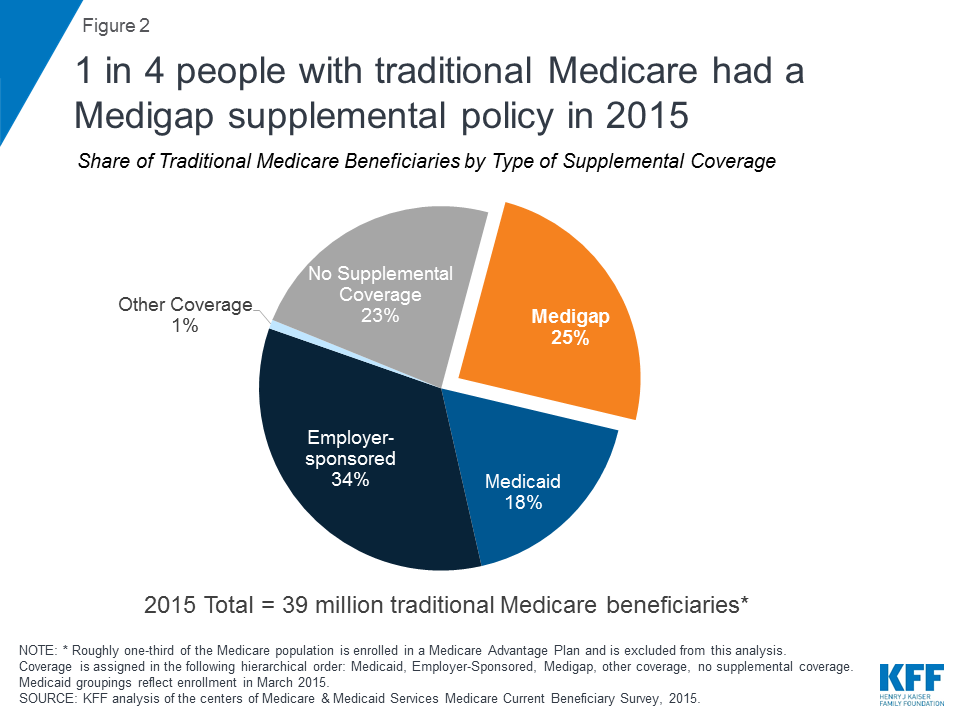
Medigap Enrollment And Consumer Protections Vary Across States Kff
Part A does not cover the following.
. Medicare was not designed for a specific class of society but primarily for. Communicate incorrect information about their plan type or use inappropriate statements like their plan is the best or highest ranked. 10 illegal Medigap practices to watch for Call the Inspector Generals hotline if you believe a federal law has been broken like if someone tries to.
At age 65 or if you have certain disabilities you become eligible for health coverage through various. Which of the following is not considered unsolicited contact with a medicare eligible consumer. D Anyone who is willing to pay a premium.
Items Services Not Covered Under Medicare MLN Booklet Page 7 of 19 ICN MLN906765 December 2020. On this page we have gathered for you the most accurate and comprehensive information that will fully answer the question. Looking for an answer to the question.
Wrong- Your answer is wrong. For which policy type is the threshold for deductibility lower after one reaches the age of 65. Steer you into a particular plan.
A private room in the hospital or a skilled nursing facility unless medically necessary. Once contact is made or 9 months from the date the consumer provided permission eg. Use of an accidental means test is prohibited.
A Anyone who qualifies through Social Security. Brokers Must Avoid These Activities During an Event or Appointment The following activities are prohibited during sales events and appointments. As an agent you must not do which of the following when marketing UnitedHealthcare Medicare Advantage plans to consumers.
Answer D is correct. Receiving full Medicaid benefits or assistance with Medicare premiums or cost sharing through one of these Medicare Savings Program MSP eligibility groups. Related MCQs All of the following are parties to a life insurance contract EXCEPT.
Medicare Advantage plans such as HMOs or PPOs must cover all the same Part B services that the original Medicare program does. Medical expense insurance and long-term care insurance. Which of the following is not considered unsolicited contact with a medicare eligible consumer.
The term includes beneficiaries enrolled in Medicare Part A Part B or both and. C Anyone over 65 not qualifying for hospital insurance and willing to pay premiums. It also prohibits an entity from presenting or causing to be presented a.
Medical expense insurance long-term care insurance and disability income insurance. All the following qualify for Medicare Part A except. False Claims Act FCA Anti-Kickback Statute AKS Physician Self-Referral Law Stark Law Social Security Act which includes the Exclusion Statute and the Civil Monetary Penalties Law CMPL United States Criminal Code.
Charge you a fee to process your enrollment into a plan. 1 Established policy requires either all services in a certain period covered or noncovered be billed together so that all such services can be bundled for payment consideration ie procedures provided on the same day. Medicare prohibits organizations from collecting donations when doing what type of billing.
Medicare Fraud and Abuse Laws. Qualified Medicare Beneficiary QMB Program. Correct- Your answer is correct.
A television or telephone in your room and personal items like razors or slipper socks unless the hospital or skilled nursing facility provides these to all patients at no additional charge. Section 1877 of the Social Security Act 42 USC. If you have ESRD you might be eligible for Medicare but you must apply for Medicare benefits by visiting your local Social Security office or contacting Social Security 1-800-772-1213 TTY users 1-800-325-0778 from 7AM 7PM Monday Friday all US.
Medicare coverage usually starts on the first day of the fourth month of your dialysis. B Anyone who was a railroad or government employee. In general Medicare doesnt cover supplies services and drugs that are not medically necessary and reasonable Medicare considers services needed for the diagnosis care and treatment of a patients condition to be medically necessary.
Conducting health screenings and similar activities that give the impression of cherry-picking Require enrollees to provide their contact information before they can attend a sales event. Billing of QMBs Is Prohibited by Federal Law Federal law bars Medicare providers and suppliers from billing an individual enrolled in the QMB program for Medicare Part A and Part B cost-sharing under any circumstances see Sections 1902n3B 1902n3C 1905p3 1866a1A and 1848g3A of the Social Security Act the Act. Pressure you to buy a Medigap policy or lie to get you to switch to a new company or policy.
Medicare does not require procedures excluded by statute to be billed on institutional claims submitted to FIAB MAC RHHIs UNLESS. Consumer signature date on BRC or 90 days if on federal do not call list whichever comes first. In order to be eligible for coverage such items must qualify in either.
Medicare has limited coverage provisions for shoes inserts and shoe modifications used by beneficiaries. Roster billing ex influenza case by case non-pars may accept assignment on case by case basis. 1395nn prohibits physicians from referring Medicare patients for certain designated health services DHS to an entity with which the physician or a member of the physicians immediate family has a financial relationship unless an exception applies.
Denies coverage of a patients overall hospital or skilled nursing facility SNF stay because its determined to be custodial care. 1 the benefit category for therapeutic shoes provisioned in the treatment of a diabetes-related conditions or 2 the benefit category for leg braces to which the shoes and related items. For instance Part B.
Sell you a second Medigap policy when they know you already have one. During the meeting Medicare plans and people who work with Medicare cant. Long-term care insurance only.
Medical expense insurance only. Julie a consumer is having difficulty understanding the information her agent Victor is presenting at her in-home appointment. Use providers or provider groups to distribute printed information comparing benefits of different health plans without approval.
Medicare is a federal benefit that you pay for through taxes during your working years. Detailed Answer C is correct. These supplies and services cannot be primarily for the convenience of the provider or beneficiary.
Medicare may cover individual reasonable and necessary services under Part B even though Part A. Helps pay premiums deductibles. Some plans for example provide coverage for routine hearing vision andor dental care fitness programs and gym memberships and emergency care abroad.
Federal laws governing Medicare fraud and abuse include the.
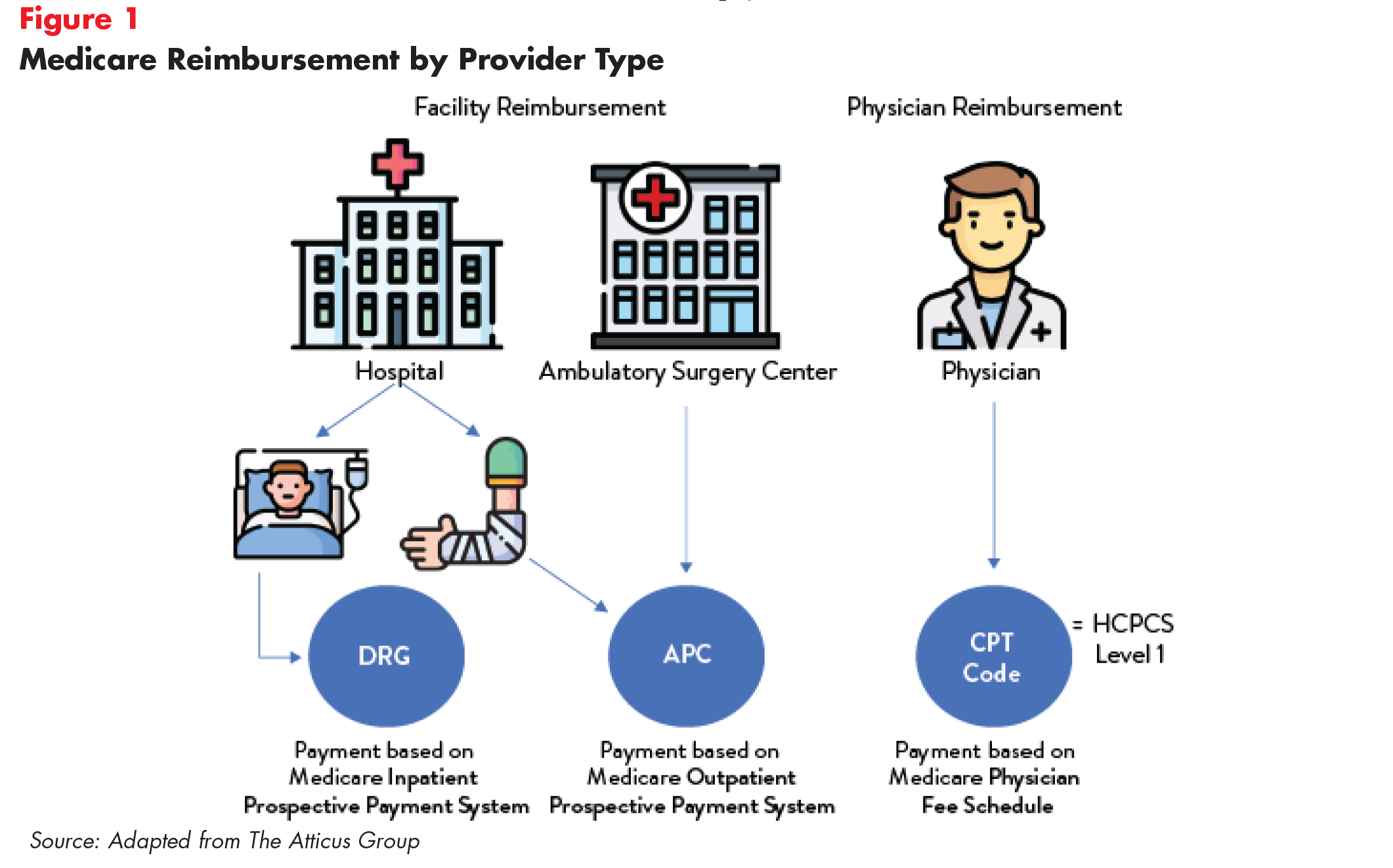
Medicare Rates As A Benchmark Too Much Too Little Or Just Right Altarum Healthcare Value Hub

Via Twitter Learn More About This Project By Clicking Through Medicare Outreach Projects Advocacy
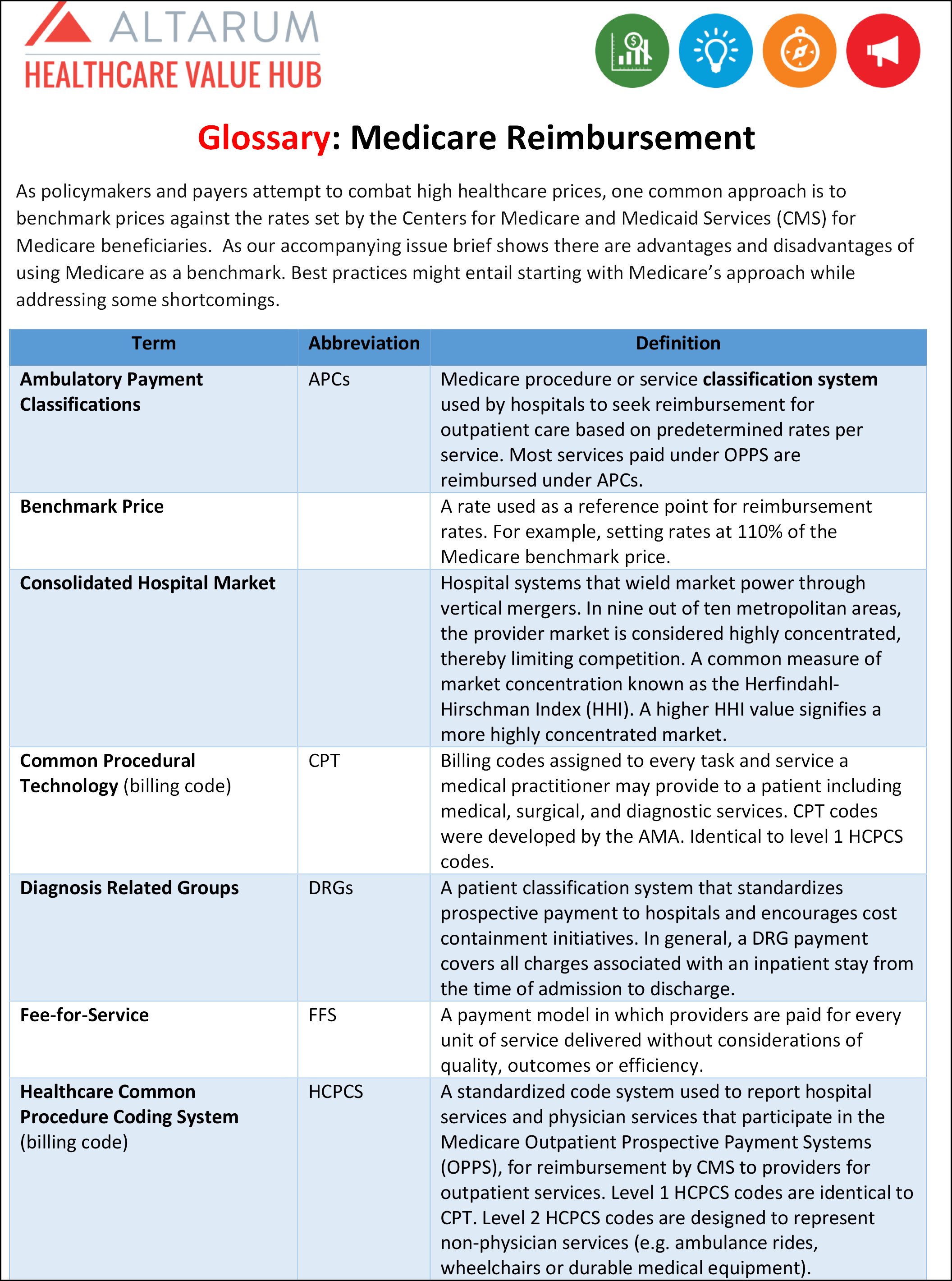
Medicare Rates As A Benchmark Too Much Too Little Or Just Right Altarum Healthcare Value Hub
No comments for "Which of the Following Is Prohibited by Medicare"
Post a Comment